Staff Perspective: Pondering the question of prescribed cannabis use and the potential effect on Trauma and Stressor-Related treatment (Part 1)
Frequently, in the past couple of years a question has emerged regarding how to handle a very specific situation in mental health treatment. That situation is what to do when a patient appropriate for PTSD treatment is also taking medicinal grade prescription cannabis for other issues such as chronic pain, anxiety or insomnia. What makes this question unique from the issue of any substance use/abuse during mental health treatment is the unknown quality of this substance. For instance, if a patient states they drink 2-3 glasses of wine approximately 3 nights a week, we have a good idea of how this substance use may affect their ability to process cognitions and emotions. However, with cannabis there are many questions.
Part 2: What do we know about the use of marijuana in the treatment of PTSD?
Is all medical-grade cannabis of the same quality? Is the THC level low enough that therapists don’t need to be concerned about patients being “high” during sessions or while doing assigned homework?
Marijuana is not a uniform product, varying considerably by strain, cultivation technique, and manner of processing. The resulting cannabis phenotypes contribute to wide variations in potency across both time and place. Interestingly, there appears to be a tendency among U.S. home cultivators toward growing higher potency medical marijuana than what is otherwise generally available.
Potency also varies on a state-by-state level, with no current federal legislation governing an overall national consistency. Currently, there are 25 states, plus the District of Columbia that have legalized use of the marijuana plant for medical purposes. This legislation differs from that for recreational use. Not included in that number are states whose legalization laws require physicians to "prescribe" marijuana (an illegal act under federal law) vs. "recommend" marijuana (considered protected free speech between doctor and patient), as well as states that have passed "affirmative defense" laws in which arrested marijuana users are allowed to mention medical use in their defense. Notably, mean potency is nearly 3.5 percentage points higher in states with a medical marijuana law. No studies have yet directly examined the effect of marijuana decriminalization on potency, which leaves clinicians and researchers able only to speculate about possible impacts.
Marijuana contains a variety of components (cannabinoids), most notably delta-9-tetrahydrocannabinol (THC) the primary psychoactive compound in the marijuana plant. Marijuana can vary in cannabinoid concentration, such as in the ratio of THC to other cannabinoids (CBD in particular). Therefore, the effects of marijuana use (e.g., experience of a high, anxiety, sleep) vary as a function of the concentration of cannabinoids (e.g., THC/CBD). In addition, the potency of cannabinoids can vary. For example, the concentration of THC in the marijuana plant can range in strength from less than 1% to 30% based upon strain and cultivation methods. In general, the potency of THC in the marijuana plant has increased as much as 10-fold over the past 40 years. Recently, cannabis extract products, such as waxes and oils, have been produced and sold in which the concentration of THC can be as high as 90%.
How does cannabis effect patients with trauma or stressor-related disorders?
Evidence suggests that large proportions of military with co-occurring substance use and PTSD drop out of treatment after only one or two sessions. It has also been stated as a possibility that some service-members using medical marijuana may be less likely to initiate specialty treatment. Two primary reasons given for this are the perceptions that medical marijuana use will be curtailed or disallowed altogether once entering treatment and/or potential trauma and stressor-related patients using prescribed cannabis feel less urgency to obtain treatment.
Some service-members use marijuana to relieve PTSD symptoms and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the effectiveness of medical marijuana for PTSD. There is no evidence at this time that marijuana is an effective treatment for PTSD.
What are the effects of cannabis on emotional awareness and cognitive reappraisal?
Emotional awareness consists of two dimensions representing (1) the extent to which one attends to emotions and (2) the extent to which one can identify and understand the type and source of emotions one experiences (i.e., emotional clarity).
Research has found that low levels of emotional awareness, and especially, low levels of emotional clarity are an independent and strong predictor of a range of psychopathology. It has also been found that low levels of emotional clarity correlate with higher levels of cannabis use.
Cognitive reappraisal is defined as an emotion regulation strategy that involves changing the trajectory of an emotional response by reinterpreting the meaning of the emotional stimulus. This technique is used in evidence-based treatments such as Cognitive Processing Therapy and in cognitive behavioral therapy for a wide variety of disorders.
When inhaled, delivered orally or transdermally, cannabinoids (the psychoactive components of unrefined marijuana and various derivative products) activate cannabinoid receptors, modulating neurotransmitter release and producing a wide range of central nervous system effects, including increased pleasure and alteration of memory processes. This can be viewed as both good news and bad news. In Part 2 of this blog we will take a closer look at the effects of cannabis use for the treatment of PTSD. Here it is important to consider how an increase in one emotion, that of pleasure, might be used as a method to avoid, numb or disregard other important emotions. Investigation to determine if the effects are temporary or longer-lasting are still being researched. When looking at the effect of an alteration in how memories are processed, it is suggested in current research that this is a temporary reprieve. Alteration in memory processing is hypothesized by several sources to be the cause of psychological reliving and continued response to triggering stimuli.
While there is research being conducted currently on this issue, there is no study of marijuana use in the Veteran population. The number of Veterans with PTSD varies by service era and is generally considered to be underreported:
- Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF): About 11-20 out of every 100 Veterans (or between 11-20%) who served in OIF or OEF have PTSD in a given year.
- Gulf War (Desert Storm): About 12 out of every 100 Gulf War Veterans (or 12%) have PTSD in a given year.
- Vietnam War: About 15 out of every 100 Vietnam Veterans (or 15%) were currently diagnosed with PTSD at the time of the most recent study in the late 1980s, the National Vietnam Veterans Readjustment Study (NVVRS). It is estimated that about 30 out of every 100 (or 30%) of Vietnam Veterans have had PTSD in their lifetime.
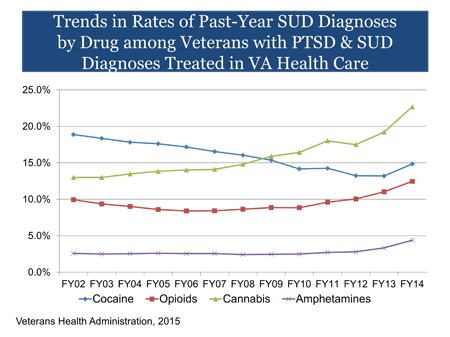
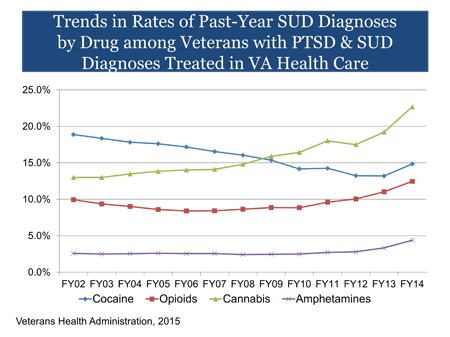
Given the number of Veterans diagnosed with PTSD, and recognizing that this number may increase exponentially by adding active duty military members, the graph below is one that clinicians need to take note of and consider how this upward trend of cannabis use impacts their treatment with patients using or being prescribed marijuana.
There is a need for a greater understanding of the benefits of cannabis and who might most reap lasting benefits for medical and psychological conditions. Additionally, it is equally important to understand the detriments of cannabis use and for what groups of individuals and diagnoses. Further, interventions may be especially important for individuals using medical cannabis to specifically cope with or “treat” medical or psychological conditions that result in emotional disturbances (e.g., anxiety disorders, depression associated with cancer). It may be important to intervene in an attempt to increase emotional clarity and the successful use of specific emotion regulation strategies among such individuals. Doing so might potentially decrease their need for medical cannabis.
Part 2: What do we know about the use of marijuana in the treatment of PTSD?
Laura Copland, MA, LCMHC is the Senior PTSD Treatment Trainer at the Center for Deployment Psychology (CDP) at Uniformed Services University of the Health Sciences in Bethesda, Maryland and a National Cognitive Processing Therapy Trainer.
References
- Boden, MT, Gross, JJ, Babson KA, Bonn-Miller MO. The interactive effects of emotional clarity and cognitive reappraisal on problematic cannabis use among medical cannabis users. Addictive Behaviors 38 (2013) 1663–1668
- Mehmedic, Z., Chandra, S., Slade, D., Denham, H., Foster, S., Patel, A. S., Ross, S. A., Khan, I. A., & Eisohly, M. A. (2010). Potency trends of Δ9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. Journal of Forensic Sciences, 55, 1209-1217. doi: 10.1111/j.1556-4029.2010.01441.x
- Sevigny, E. L., Pacula, R. L., & Heaton, P. (2014) The effects of medical marijuana laws on potency. International Journal of Drug Policy, 25, 308-319. doi: 10.1016/j.drugpo.2014.01.003
- Bonn-Miller MO, Vujanovic AA, Boden MT et al. Post-traumatic stress, difficulties in emotion regulation, and coping oriented marijuana use. Cogn Behav Ther.2011; 40:34-44.
- Bonn-Miller MO, Vujanovic AA, Feldner MT et al. Post-traumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. J Trauma Stress. 2007; 20:577-86.
- Potter CM, Vujanovic AA, Marshall-Berenz EC et al. Post-traumatic stress and marijuana use coping motives: the mediating role of distress tolerance. J Anxiety Disord. 2011; 25:437-43.
- Bonn-Miller MO, Rousseau, GS (2016). Marijuana Use and PTSD among Veterans. National Center for PTSD.
- NYU Langione Medical Center. “Brain-imaging study links cannabinoid receptors to post-traumatic stress disorder: First pharmaceutical treatment for PTSD within reach.” ScienceDaily, 14 May 2013. www.sciencedaily.com/releases/2013/05/130514085016.htm
- Gannon-Elazar E, Akirav I (2009). Cannabinoid Receptor Activation in the Basolateral Amygdala Blocks the Effects of Stress on the Conditioning and Extinction of Inhibitory Avoidance. Journal of Neuroscience. 9 September 2009, 29(36).
Part 2: What do we know about the use of marijuana in the treatment of PTSD?
Frequently, in the past couple of years a question has emerged regarding how to handle a very specific situation in mental health treatment. That situation is what to do when a patient appropriate for PTSD treatment is also taking medicinal grade prescription cannabis for other issues such as chronic pain, anxiety or insomnia. What makes this question unique from the issue of any substance use/abuse during mental health treatment is the unknown quality of this substance. For instance, if a patient states they drink 2-3 glasses of wine approximately 3 nights a week, we have a good idea of how this substance use may affect their ability to process cognitions and emotions. However, with cannabis there are many questions.
Part 2: What do we know about the use of marijuana in the treatment of PTSD?
Is all medical-grade cannabis of the same quality? Is the THC level low enough that therapists don’t need to be concerned about patients being “high” during sessions or while doing assigned homework?
Marijuana is not a uniform product, varying considerably by strain, cultivation technique, and manner of processing. The resulting cannabis phenotypes contribute to wide variations in potency across both time and place. Interestingly, there appears to be a tendency among U.S. home cultivators toward growing higher potency medical marijuana than what is otherwise generally available.
Potency also varies on a state-by-state level, with no current federal legislation governing an overall national consistency. Currently, there are 25 states, plus the District of Columbia that have legalized use of the marijuana plant for medical purposes. This legislation differs from that for recreational use. Not included in that number are states whose legalization laws require physicians to "prescribe" marijuana (an illegal act under federal law) vs. "recommend" marijuana (considered protected free speech between doctor and patient), as well as states that have passed "affirmative defense" laws in which arrested marijuana users are allowed to mention medical use in their defense. Notably, mean potency is nearly 3.5 percentage points higher in states with a medical marijuana law. No studies have yet directly examined the effect of marijuana decriminalization on potency, which leaves clinicians and researchers able only to speculate about possible impacts.
Marijuana contains a variety of components (cannabinoids), most notably delta-9-tetrahydrocannabinol (THC) the primary psychoactive compound in the marijuana plant. Marijuana can vary in cannabinoid concentration, such as in the ratio of THC to other cannabinoids (CBD in particular). Therefore, the effects of marijuana use (e.g., experience of a high, anxiety, sleep) vary as a function of the concentration of cannabinoids (e.g., THC/CBD). In addition, the potency of cannabinoids can vary. For example, the concentration of THC in the marijuana plant can range in strength from less than 1% to 30% based upon strain and cultivation methods. In general, the potency of THC in the marijuana plant has increased as much as 10-fold over the past 40 years. Recently, cannabis extract products, such as waxes and oils, have been produced and sold in which the concentration of THC can be as high as 90%.
How does cannabis effect patients with trauma or stressor-related disorders?
Evidence suggests that large proportions of military with co-occurring substance use and PTSD drop out of treatment after only one or two sessions. It has also been stated as a possibility that some service-members using medical marijuana may be less likely to initiate specialty treatment. Two primary reasons given for this are the perceptions that medical marijuana use will be curtailed or disallowed altogether once entering treatment and/or potential trauma and stressor-related patients using prescribed cannabis feel less urgency to obtain treatment.
Some service-members use marijuana to relieve PTSD symptoms and several states specifically approve the use of medical marijuana for PTSD. However, controlled studies have not been conducted to evaluate the effectiveness of medical marijuana for PTSD. There is no evidence at this time that marijuana is an effective treatment for PTSD.
What are the effects of cannabis on emotional awareness and cognitive reappraisal?
Emotional awareness consists of two dimensions representing (1) the extent to which one attends to emotions and (2) the extent to which one can identify and understand the type and source of emotions one experiences (i.e., emotional clarity).
Research has found that low levels of emotional awareness, and especially, low levels of emotional clarity are an independent and strong predictor of a range of psychopathology. It has also been found that low levels of emotional clarity correlate with higher levels of cannabis use.
Cognitive reappraisal is defined as an emotion regulation strategy that involves changing the trajectory of an emotional response by reinterpreting the meaning of the emotional stimulus. This technique is used in evidence-based treatments such as Cognitive Processing Therapy and in cognitive behavioral therapy for a wide variety of disorders.
When inhaled, delivered orally or transdermally, cannabinoids (the psychoactive components of unrefined marijuana and various derivative products) activate cannabinoid receptors, modulating neurotransmitter release and producing a wide range of central nervous system effects, including increased pleasure and alteration of memory processes. This can be viewed as both good news and bad news. In Part 2 of this blog we will take a closer look at the effects of cannabis use for the treatment of PTSD. Here it is important to consider how an increase in one emotion, that of pleasure, might be used as a method to avoid, numb or disregard other important emotions. Investigation to determine if the effects are temporary or longer-lasting are still being researched. When looking at the effect of an alteration in how memories are processed, it is suggested in current research that this is a temporary reprieve. Alteration in memory processing is hypothesized by several sources to be the cause of psychological reliving and continued response to triggering stimuli.
While there is research being conducted currently on this issue, there is no study of marijuana use in the Veteran population. The number of Veterans with PTSD varies by service era and is generally considered to be underreported:
- Operations Iraqi Freedom (OIF) and Enduring Freedom (OEF): About 11-20 out of every 100 Veterans (or between 11-20%) who served in OIF or OEF have PTSD in a given year.
- Gulf War (Desert Storm): About 12 out of every 100 Gulf War Veterans (or 12%) have PTSD in a given year.
- Vietnam War: About 15 out of every 100 Vietnam Veterans (or 15%) were currently diagnosed with PTSD at the time of the most recent study in the late 1980s, the National Vietnam Veterans Readjustment Study (NVVRS). It is estimated that about 30 out of every 100 (or 30%) of Vietnam Veterans have had PTSD in their lifetime.
Given the number of Veterans diagnosed with PTSD, and recognizing that this number may increase exponentially by adding active duty military members, the graph below is one that clinicians need to take note of and consider how this upward trend of cannabis use impacts their treatment with patients using or being prescribed marijuana.
There is a need for a greater understanding of the benefits of cannabis and who might most reap lasting benefits for medical and psychological conditions. Additionally, it is equally important to understand the detriments of cannabis use and for what groups of individuals and diagnoses. Further, interventions may be especially important for individuals using medical cannabis to specifically cope with or “treat” medical or psychological conditions that result in emotional disturbances (e.g., anxiety disorders, depression associated with cancer). It may be important to intervene in an attempt to increase emotional clarity and the successful use of specific emotion regulation strategies among such individuals. Doing so might potentially decrease their need for medical cannabis.
Part 2: What do we know about the use of marijuana in the treatment of PTSD?
Laura Copland, MA, LCMHC is the Senior PTSD Treatment Trainer at the Center for Deployment Psychology (CDP) at Uniformed Services University of the Health Sciences in Bethesda, Maryland and a National Cognitive Processing Therapy Trainer.
References
- Boden, MT, Gross, JJ, Babson KA, Bonn-Miller MO. The interactive effects of emotional clarity and cognitive reappraisal on problematic cannabis use among medical cannabis users. Addictive Behaviors 38 (2013) 1663–1668
- Mehmedic, Z., Chandra, S., Slade, D., Denham, H., Foster, S., Patel, A. S., Ross, S. A., Khan, I. A., & Eisohly, M. A. (2010). Potency trends of Δ9-THC and other cannabinoids in confiscated cannabis preparations from 1993 to 2008. Journal of Forensic Sciences, 55, 1209-1217. doi: 10.1111/j.1556-4029.2010.01441.x
- Sevigny, E. L., Pacula, R. L., & Heaton, P. (2014) The effects of medical marijuana laws on potency. International Journal of Drug Policy, 25, 308-319. doi: 10.1016/j.drugpo.2014.01.003
- Bonn-Miller MO, Vujanovic AA, Boden MT et al. Post-traumatic stress, difficulties in emotion regulation, and coping oriented marijuana use. Cogn Behav Ther.2011; 40:34-44.
- Bonn-Miller MO, Vujanovic AA, Feldner MT et al. Post-traumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. J Trauma Stress. 2007; 20:577-86.
- Potter CM, Vujanovic AA, Marshall-Berenz EC et al. Post-traumatic stress and marijuana use coping motives: the mediating role of distress tolerance. J Anxiety Disord. 2011; 25:437-43.
- Bonn-Miller MO, Rousseau, GS (2016). Marijuana Use and PTSD among Veterans. National Center for PTSD.
- NYU Langione Medical Center. “Brain-imaging study links cannabinoid receptors to post-traumatic stress disorder: First pharmaceutical treatment for PTSD within reach.” ScienceDaily, 14 May 2013. www.sciencedaily.com/releases/2013/05/130514085016.htm
- Gannon-Elazar E, Akirav I (2009). Cannabinoid Receptor Activation in the Basolateral Amygdala Blocks the Effects of Stress on the Conditioning and Extinction of Inhibitory Avoidance. Journal of Neuroscience. 9 September 2009, 29(36).
Part 2: What do we know about the use of marijuana in the treatment of PTSD?

