By the Numbers - Oct. 31, 2016
48.1%
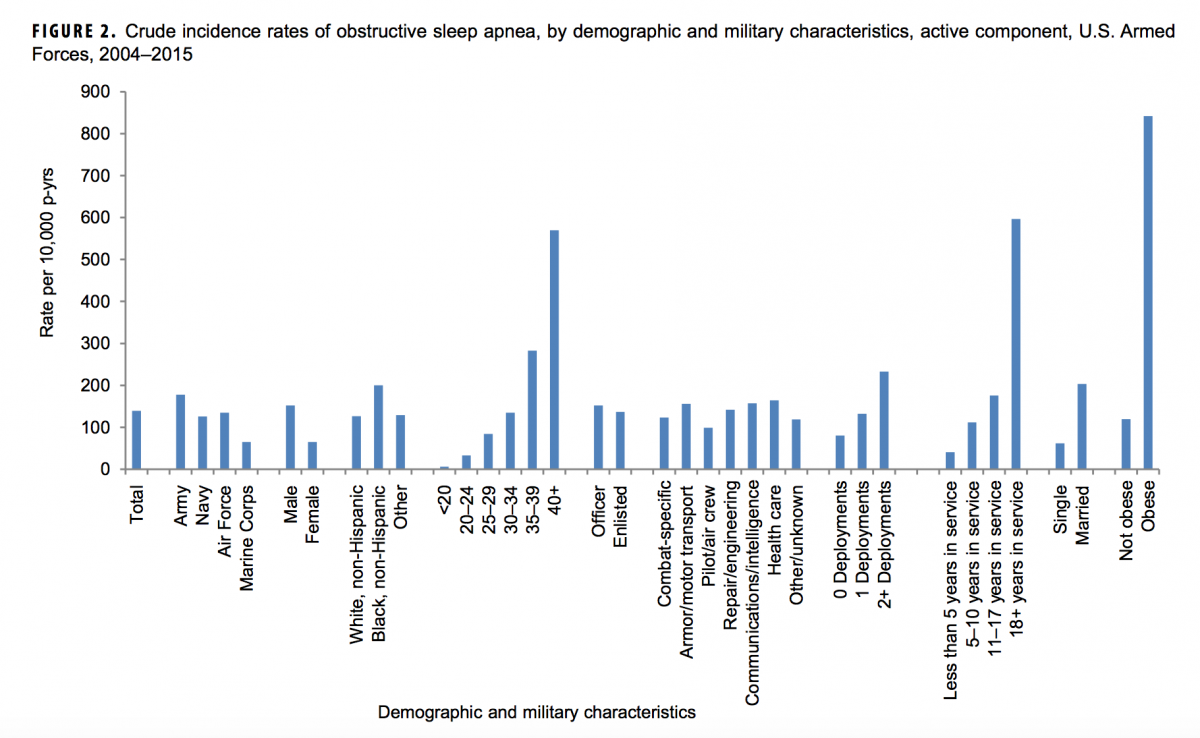
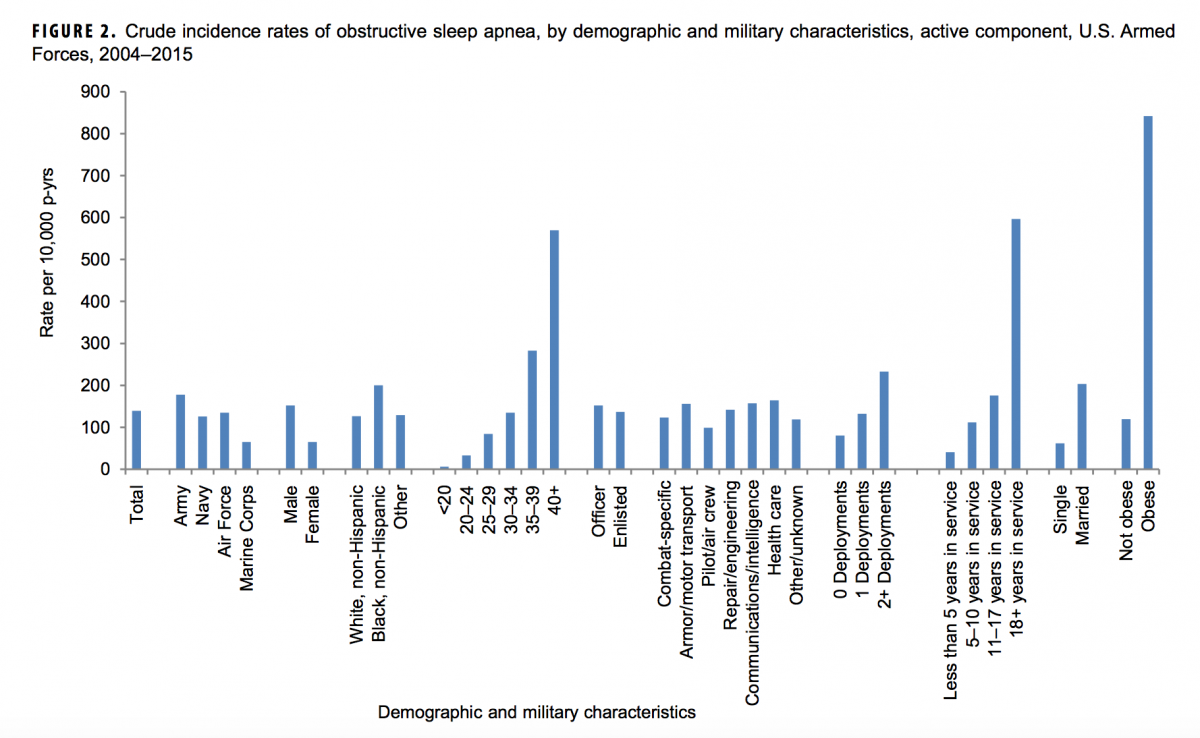
The percentage of obstructive sleep apnea (OSA) cases among "active component military members" that are diagnosed in the last year of service, according to a report in the October issue of the Armed Forces Health Surveillance Branch monthly publication, Medical Surveillance Monthly Report -- Obstructive Sleep Apnea and Associated Attrition, Active Component, U.S. Armed Forces, January 2004–May 2016. According to the report:
OSA is defined clinically as the complete or near complete cessation of airflow during sleep due to the obstruction of the upper airway. Individuals with OSA may suffer symptoms such as snoring, gasping for breath during sleep, insomnia, headaches, and daytime fatigue. Individuals who suffer from OSA have increased rates of motor vehicle accidents, cardio-vascular disease (including stroke and high blood pressure), diabetes, and cognitive impairment.
The researchers indicate that OSA "is a growing health concern in both civilian and military populations," but it's an especially critical issue for the armed services.
A diagnosis of OSA requiring a CPAP machine is classified as a 50% Military Disability Rating. It is estimated that the VA’s yearly compensation costs for OSA will exceed $1 billion due to the MDB alone. The true cost to the DoD and VA is likely underestimated, as diagnosis and treatment are only 3% of the total economic burden of OSA. The proportion of hidden costs including loss of work productivity and comorbid medical conditions may be even higher in the DoD population, compared to civilian populations, because of the unique military mission utilizing expensive equipment and the dangerous situations in which service members must operate.
The high percentage of cases diagnosed prior to separation from service is concerning because OSA is a treatable and partially preventable disease. OSA represents a large health and economic burden for the armed services and yet there are persistent research gaps in appropriate screening and prevention strategies to improve both individual health and mission performance.
MSMR, Vol. 23 No. 10 October 2016, p. 7
48.1%
The percentage of obstructive sleep apnea (OSA) cases among "active component military members" that are diagnosed in the last year of service, according to a report in the October issue of the Armed Forces Health Surveillance Branch monthly publication, Medical Surveillance Monthly Report -- Obstructive Sleep Apnea and Associated Attrition, Active Component, U.S. Armed Forces, January 2004–May 2016. According to the report:
OSA is defined clinically as the complete or near complete cessation of airflow during sleep due to the obstruction of the upper airway. Individuals with OSA may suffer symptoms such as snoring, gasping for breath during sleep, insomnia, headaches, and daytime fatigue. Individuals who suffer from OSA have increased rates of motor vehicle accidents, cardio-vascular disease (including stroke and high blood pressure), diabetes, and cognitive impairment.
The researchers indicate that OSA "is a growing health concern in both civilian and military populations," but it's an especially critical issue for the armed services.
A diagnosis of OSA requiring a CPAP machine is classified as a 50% Military Disability Rating. It is estimated that the VA’s yearly compensation costs for OSA will exceed $1 billion due to the MDB alone. The true cost to the DoD and VA is likely underestimated, as diagnosis and treatment are only 3% of the total economic burden of OSA. The proportion of hidden costs including loss of work productivity and comorbid medical conditions may be even higher in the DoD population, compared to civilian populations, because of the unique military mission utilizing expensive equipment and the dangerous situations in which service members must operate.
The high percentage of cases diagnosed prior to separation from service is concerning because OSA is a treatable and partially preventable disease. OSA represents a large health and economic burden for the armed services and yet there are persistent research gaps in appropriate screening and prevention strategies to improve both individual health and mission performance.
MSMR, Vol. 23 No. 10 October 2016, p. 7