Staff Perspective: Weeding Through the Literature on Marijuana Use in Treating PTSD (Part 2)
In Part 1 of this blog titled, Pondering the Question of Prescribed Cannabis Use and the Potential Effect on Trauma and Stressor-Related Treatment, I closed by saying that while research is being conducted currently on this issue, there is no study of marijuana use in the Veteran population. I am happy to report that research with 76 Veteran participants who have treatment-resistant PTSD was approved by the DEA and is underway. As reported in The Military Times, April 2016 edition, the study will use marijuana of various strains and potency for comparison purposes. This will be the first randomized, controlled research in the U.S. for PTSD that will use the actual plant instead of oils or synthesized cannabis. The University of Pennsylvania Perelman School of Medicine and Johns Hopkins University will be overseeing the project.
While there is much anecdotal evidence among Veterans suggesting that the use of medical marijuana helps alleviate PTSD symptoms and has helped them reduce or stop using prescribed and/or non-prescribed medications, there is very little scientific research to support these claims. This new research will fill a gap in the medical literature, allowing clinicians more information on how to work with patients using cannabis for medical and psychological issues.
"This is a critical step in moving our botanical drug development program forward at the federal level to gather information on the dosing, risks, and benefits of smoked marijuana for PTSD symptoms," said Amy Emerson, director of clinical research for the MAPS Public Benefit Corporation.
That’s great news and will be helpful in the future. But what do we currently understand about the effects of marijuana on PTSD symptoms?
The literature is dense with important technical understandings, but for the purposes of this writing, I have made every attempt to condense this information for two reasons: 1) to provide just enough information to make sense of the research results and 2) so that we might use this information to talk about this issue with patients without overwhelming them.
In a reading of the scientific literature regarding the effects of cannabis and cannabinoids, one point becomes evident: cannabis has a profound influence on the human body. This one herb and its variety of therapeutic compounds seem to affect every aspect of our bodies and minds. In short, scientists studying the effects of marijuana have made several important discoveries. Not only did they identify the active ingredient in marijuana, they also discovered where and how it works in the brain—via a new system they called the endocannabinoid (EC) system. This system was discovered in the mid-1990s by Israeli researcher, Dr. Ralph Mechoulam, who also identified THC as the main active ingredient in cannabis in the early 1960s. Israel has been one of the most progressive nations for cannabis research and currently has one of the most advanced medical marijuana programs in the world. The EC system—named after the marijuana plant Cannabis sativa and its active ingredient THC—is a unique communications system in the brain and body that affects many important functions, including how a person feels, moves, and reacts.
THC moderates pain in that by reducing the intensity of the pain in the cannabis receptor 1 (CB1) site. This mechanism of action is why THC-rich medicines are being prescribe for and used by people with intense, chronic pain issues. Cannabis and narcotics are also co-agonists, which means that each of them magnifies the effect of the other. This allows people to take lower doses of narcotics and still have it be effective. Additionally, CB1 receptors are not present in the part of the brain that regulates heart rate and respiration, so unlike narcotics, there is no lethal dosage threshold for THC, allowing someone to consume as much is needed for its palliative effects.
In general, cannabinoids function like a “dimmer switch” for presynaptic neurons, limiting the amount of neurotransmitter (e.g., dopamine) that gets released, which in turn affects how messages are sent, received, and processed by the cell.
The research literature has consistently demonstrated that the human cannabinoid system plays a significant role in PTSD. Specifically, the EC system is significant in people with PTSD who appear to have greater availability to CB1 receptors than healthy controls. This suggests that the use of marijuana by individuals with PTSD may help in alleviating PTSD symptoms. However, data also suggests that continued use over time may lead to marijuana tolerance and addiction since people with PTSD may have greater difficulty quitting than those without a PTSD diagnosis.
In a 2009 Israeli study published in The Journal of Neuroscience and using 434 rats as subjects, the, the primary goal was to test whether cannabinoid activation of the amygdala (see amygdala in diagram below) would inhibit stress-induced alterations in avoidance, stress and memory extinction, specifically, those symptoms of inappropriate retention of aversive memories leading to PTSD. Their conclusions are promising and give support to the suggestion that marijuana may represent a therapeutic tool in targeting PTSD symptoms.
The study did suggest, however, that marijuana may have adverse effects on accessing emotions with the drug-induced creation of euphoria and a general feeling of well-being. This then suggests that the dose together with the context of administration should be taken into consideration when being prescribed and could possibly block aspects of evidence-based treatment options such as Prolonged Exposure (PE) or Cognitive Processing Therapy (CPT).
A study published in 2014, “PTSD Symptom Reports of Patients Evaluated for the New Mexico Medical Cannabis Program” by George Greer, et al found that although currently there is no substantial proof of the efficacy of cannabis in PTSD treatment, the data reviewed supports a conclusion that cannabis is associated with PTSD symptom reduction in some patients.
The conclusion, at this time, is that evidence suggests the use of marijuana is helpful for PTSD symptom reduction such as trauma memory retention, anxiety and hyperarousal. As I mentioned in Part I of this blog, the issues of unknown dosage and the effects of the variety of administrations continues to prevent clinicians from providing more than an educated guess about how marijuana will impact PTSD treatment. Clinicians should candidly discuss marijuana use with their patients and offer education about potential problems with long-term marijuana use. Although it appears that marijuana may have some positive attributes for those with PTSD, with the current limited knowledge, it is wise to proceed with caution at this juncture of awareness.
Locations of Cannabinoid Receptors in the Brain
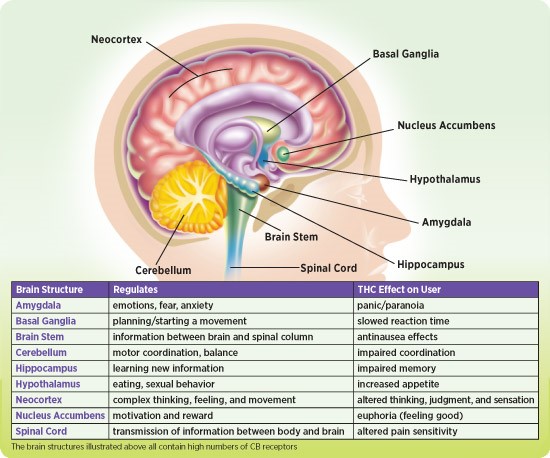
From Scholastic, Inc. and the Scientists of the National Institute of Drug Abuse, National Institutes of Health, U.S. Department of Health and Human Services.
Laura Copland, MA, LCMHC is the Senior PTSD Treatment Trainer at the Center for Deployment Psychology (CDP) at Uniformed Services University of the Health Sciences in Bethesda, Maryland and a National Cognitive Processing Therapy Trainer.
In Part 1 of this blog titled, Pondering the Question of Prescribed Cannabis Use and the Potential Effect on Trauma and Stressor-Related Treatment, I closed by saying that while research is being conducted currently on this issue, there is no study of marijuana use in the Veteran population. I am happy to report that research with 76 Veteran participants who have treatment-resistant PTSD was approved by the DEA and is underway. As reported in The Military Times, April 2016 edition, the study will use marijuana of various strains and potency for comparison purposes. This will be the first randomized, controlled research in the U.S. for PTSD that will use the actual plant instead of oils or synthesized cannabis. The University of Pennsylvania Perelman School of Medicine and Johns Hopkins University will be overseeing the project.
While there is much anecdotal evidence among Veterans suggesting that the use of medical marijuana helps alleviate PTSD symptoms and has helped them reduce or stop using prescribed and/or non-prescribed medications, there is very little scientific research to support these claims. This new research will fill a gap in the medical literature, allowing clinicians more information on how to work with patients using cannabis for medical and psychological issues.
"This is a critical step in moving our botanical drug development program forward at the federal level to gather information on the dosing, risks, and benefits of smoked marijuana for PTSD symptoms," said Amy Emerson, director of clinical research for the MAPS Public Benefit Corporation.
That’s great news and will be helpful in the future. But what do we currently understand about the effects of marijuana on PTSD symptoms?
The literature is dense with important technical understandings, but for the purposes of this writing, I have made every attempt to condense this information for two reasons: 1) to provide just enough information to make sense of the research results and 2) so that we might use this information to talk about this issue with patients without overwhelming them.
In a reading of the scientific literature regarding the effects of cannabis and cannabinoids, one point becomes evident: cannabis has a profound influence on the human body. This one herb and its variety of therapeutic compounds seem to affect every aspect of our bodies and minds. In short, scientists studying the effects of marijuana have made several important discoveries. Not only did they identify the active ingredient in marijuana, they also discovered where and how it works in the brain—via a new system they called the endocannabinoid (EC) system. This system was discovered in the mid-1990s by Israeli researcher, Dr. Ralph Mechoulam, who also identified THC as the main active ingredient in cannabis in the early 1960s. Israel has been one of the most progressive nations for cannabis research and currently has one of the most advanced medical marijuana programs in the world. The EC system—named after the marijuana plant Cannabis sativa and its active ingredient THC—is a unique communications system in the brain and body that affects many important functions, including how a person feels, moves, and reacts.
THC moderates pain in that by reducing the intensity of the pain in the cannabis receptor 1 (CB1) site. This mechanism of action is why THC-rich medicines are being prescribe for and used by people with intense, chronic pain issues. Cannabis and narcotics are also co-agonists, which means that each of them magnifies the effect of the other. This allows people to take lower doses of narcotics and still have it be effective. Additionally, CB1 receptors are not present in the part of the brain that regulates heart rate and respiration, so unlike narcotics, there is no lethal dosage threshold for THC, allowing someone to consume as much is needed for its palliative effects.
In general, cannabinoids function like a “dimmer switch” for presynaptic neurons, limiting the amount of neurotransmitter (e.g., dopamine) that gets released, which in turn affects how messages are sent, received, and processed by the cell.
The research literature has consistently demonstrated that the human cannabinoid system plays a significant role in PTSD. Specifically, the EC system is significant in people with PTSD who appear to have greater availability to CB1 receptors than healthy controls. This suggests that the use of marijuana by individuals with PTSD may help in alleviating PTSD symptoms. However, data also suggests that continued use over time may lead to marijuana tolerance and addiction since people with PTSD may have greater difficulty quitting than those without a PTSD diagnosis.
In a 2009 Israeli study published in The Journal of Neuroscience and using 434 rats as subjects, the, the primary goal was to test whether cannabinoid activation of the amygdala (see amygdala in diagram below) would inhibit stress-induced alterations in avoidance, stress and memory extinction, specifically, those symptoms of inappropriate retention of aversive memories leading to PTSD. Their conclusions are promising and give support to the suggestion that marijuana may represent a therapeutic tool in targeting PTSD symptoms.
The study did suggest, however, that marijuana may have adverse effects on accessing emotions with the drug-induced creation of euphoria and a general feeling of well-being. This then suggests that the dose together with the context of administration should be taken into consideration when being prescribed and could possibly block aspects of evidence-based treatment options such as Prolonged Exposure (PE) or Cognitive Processing Therapy (CPT).
A study published in 2014, “PTSD Symptom Reports of Patients Evaluated for the New Mexico Medical Cannabis Program” by George Greer, et al found that although currently there is no substantial proof of the efficacy of cannabis in PTSD treatment, the data reviewed supports a conclusion that cannabis is associated with PTSD symptom reduction in some patients.
The conclusion, at this time, is that evidence suggests the use of marijuana is helpful for PTSD symptom reduction such as trauma memory retention, anxiety and hyperarousal. As I mentioned in Part I of this blog, the issues of unknown dosage and the effects of the variety of administrations continues to prevent clinicians from providing more than an educated guess about how marijuana will impact PTSD treatment. Clinicians should candidly discuss marijuana use with their patients and offer education about potential problems with long-term marijuana use. Although it appears that marijuana may have some positive attributes for those with PTSD, with the current limited knowledge, it is wise to proceed with caution at this juncture of awareness.
Locations of Cannabinoid Receptors in the Brain
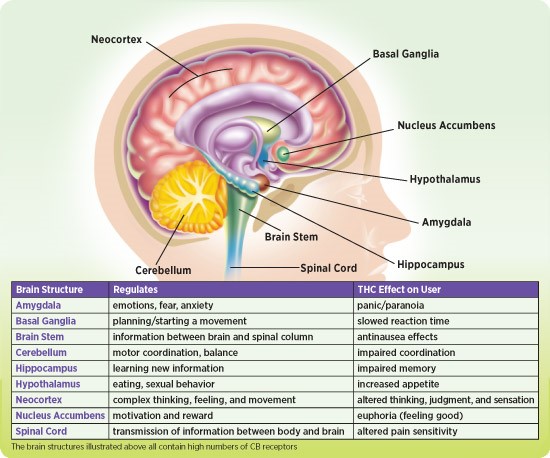
From Scholastic, Inc. and the Scientists of the National Institute of Drug Abuse, National Institutes of Health, U.S. Department of Health and Human Services.
Laura Copland, MA, LCMHC is the Senior PTSD Treatment Trainer at the Center for Deployment Psychology (CDP) at Uniformed Services University of the Health Sciences in Bethesda, Maryland and a National Cognitive Processing Therapy Trainer.

