Staff Perspective: An App for Providers, Helping Us in Sustaining Self-Care and Resiliency
It seems like everyone is carrying a smartphone these days. Some of the attributes that make these devices an asset to therapy include they’re portable, acceptable, always on (this benefit is probably up for discussion), low cost, programmable, audio and video output, user-friendliness, and ease of use (Boschen, 2008). More and more we are able to recommend and guide our patients through various evidence-based psychotherapies (EBPs) with the help of evidence-based mobile health applications or so-called “apps”. These apps, such as CBT-i Coach and CPT Coach, can supplement our sessions and make it easier for patients to record things such as sleep diaries or thought logs without the burden of remembering to carry around worksheets or journals. It can be difficult for patients to remember to do their homework and to find a place that they feel is safe enough to record their thoughts or behaviors. The accessibility and convenience of apps seems to make it that much easier for patients to engage in treatment and follow through with treatment assignments.
For providers, we now have the same accessibility of a tool that can help us implement self-care practices in our day. We understand the potential consequences of difficulty in managing stressors and the buildup for compassion fatigue, burnout, and secondary traumatic stress, in addition to the negative impact it can have on our personal and professional lives. For many, finding the time for regular self-care through such routines as meditation, yoga, exercise, proper diet, continuing education, or socializing can be difficult to maintain. With a recent development of the Provider Resilience Mobile Application, providers may find another option of implementing and sustaining self-care practices.
The Provider Resilience app, the first app focused on building resilience for health care providers, was developed by the Defense Department’s National Center for Telehealth and Technology (T2). The app allows providers to complete self-assessments of the Professional Quality of Life Scale (ProQOL), to help providers measure their level of burnout and secondary traumatic stress as well as compassion satisfaction.
Let’s take a look at a few screenshots of the app. (You can click on any of the images to see a larger version.) Here is the dashboard, where a provider can find their resilience rating. The resilience rating is based on the ProQOL and burnout score, and responses to the reduction or building of resilience, in addition to the date of your last vacation day. Yes, it also reminds providers to take time off of work. The ProQOL is updated every 30 days while the burnout rating is updated every seven days.
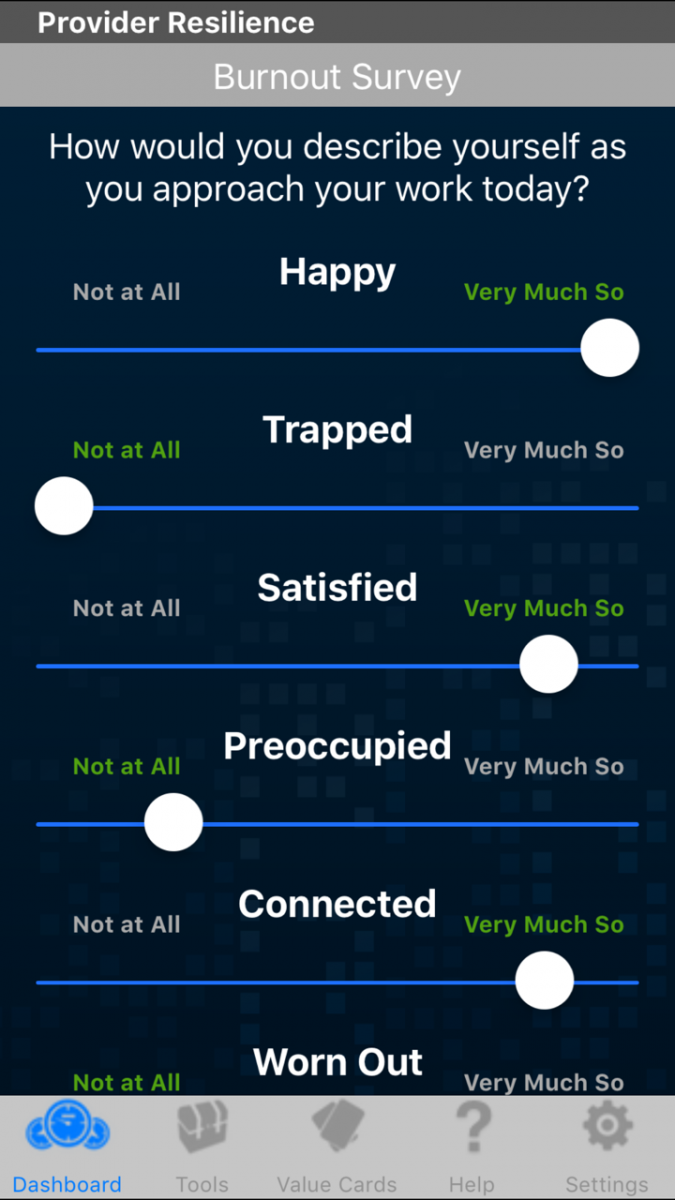
Burnout can also be tracked through provider ratings based on ten affective domains, shown here, describing your approach to work today.
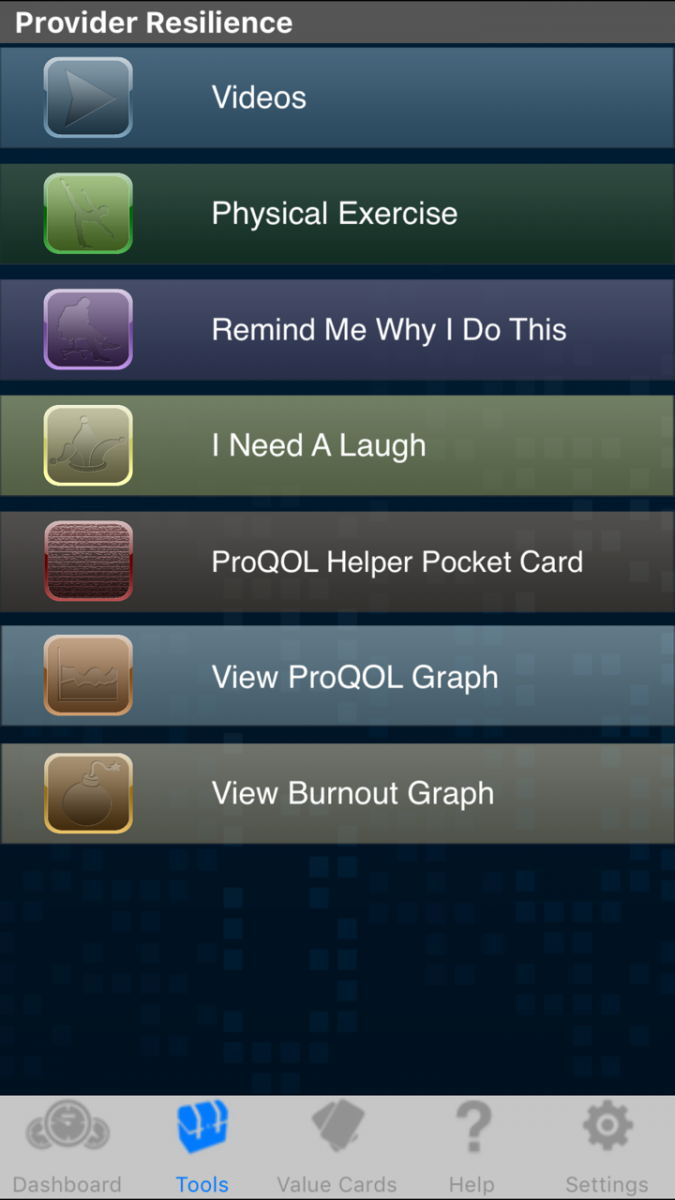 If a provider’s resilience score is low or when looking for strategies to sustain resilience, the app offers a toolbox. These include reminders to take breaks or review positive aspects of work as well as hearing Service members discuss the impact providers have on their lives. This is a great feature; the app specifically focuses on providers who serve Veterans, Service members, and their families.
If a provider’s resilience score is low or when looking for strategies to sustain resilience, the app offers a toolbox. These include reminders to take breaks or review positive aspects of work as well as hearing Service members discuss the impact providers have on their lives. This is a great feature; the app specifically focuses on providers who serve Veterans, Service members, and their families.
Providers can choose from a wide variety of options for self-care, as well as track their ratings over time on the charts.
Here are examples of the Value Cards and Exercises that providers are offered to help increase resilience. 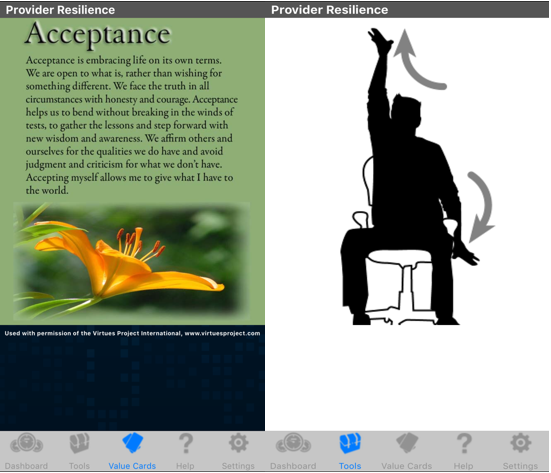
With the development of the Provider Resilience app, we can read up on the latest literature recommending an app’s effectiveness. Recently, Woods et al. (2017), completed a pilot study with 30 outpatient mental health providers who utilized Provider Resilience for a month to examine the usability and effectiveness of the app in reducing provider burnout. The researchers found that not only was the usability considered to be in the “excellent” range with users, but also there was a reduction in burnout (d=0.68) and compassion fatigue (d=0.84). Despite the small sample size, the results are promising in helping to build provider resilience.
There have also been several recent randomized controlled trials (RCT) and reviews suggesting the promising potential of how effective and useful apps are toward psychotherapeutic treatment. One randomized controlled trial (RCT) examined the impact of acceptance and commitment-based apps on stress management which demonstrated the benefits of stress interventions with mobile apps. The use of the app reduced stress and increased general health in middle managers (Ly, Asplund, & Andersson, 2014). Another RCT demonstrated how apps using either behavioral activation or mindfulness might would work well for a depressed population (Ly, et al., 2017). More so, Kuhn et al. (2017) were the first to rigorously evaluate the efficacy of a mobile app for PTSD, PTSD Coach. The results suggested that the app has a potential in helping trauma survivors with PTSD including a recommendation as a first step for those who are not receiving mental health care. A review of evidence-based apps for stress management indicated the great potential for apps in supplementing care (Coulon, Monroe, & West, 2016). Another systematic review concluded that apps are beneficial, feasible, and acceptable for a wide range of psychiatric conditions (Menson, Rajan, & Sarkar, 2017).
Having multiple options for self-care may further help to support providers in sustaining their resilience to continue to service their patients. Providers now have an easy to use app that can help increase resilience by improving levels of burnout and compassion satisfaction. When it may not be as convenient to venture outdoors or be device free, the Provider Resilience app is one more tool among the many that providers can implement into their day. These technological advances are an exciting benefit that will continue to change how we practice both our clinical and self-care tools.
Laura Cho-Stutler, PsyD, is a CBT Trainer working with the Military Training Programs at the Center for Deployment Psychology (CDP) at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
References
Boschen, M.J. (2008). The use of mobile telephones as adjuncts to Cognitive Behavioral Psychotherapy. Professional Psychology: Research and Practice, 39 (5), 546-552. DOI: 10.1037/0735-7028.39.5.546
Coulon, S.M., Monroe, C.M., West, D.S. (2016). A systemic, multi-domain review of mobile smartphone apps for evidence-based stress management. American Journal of Preventative Medicine, 51(1), 95-101. http://doi.org/10.1016/j.amepre.2016.01.026
Ly, K. H., Asplund, K., & Andersson, G. (2014). Stress management for middle managers via an acceptance and commitment-based smartphone application: A randomized controlled trial. Internet Interventions, Advance online publication. DOI: 10.1016/j.invent.2014.06.003
Ly, K. H., Trüschel, A., Jarl, L., Magnusson, S., Windahl, T., Johansson, R., & Andersson, G. (2014). Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: A randomised controlled trial. BMJ Open, 4, e003440. DOI: 10.1136/bmjopen-2013-003440
Menson, V., Rajan, T., Sarkar, S. (2017). Psychotherapeutic applications of mobile phone-based technologies: A systematic review of current research and trends. Indian Journal of Psychological Medicine, 39(1),4.
Provider Resilience. National Center for Telehealth & Technology (T2). Provider Resilience, http://t2health.dcoe.mil/apps/provider-resilience, accessed 13 April 2017.
Wood, A.E., Prins, A., Brush, N.E., Hsia, J.F., Bourn, L.E., Earley, M.D., Walser, R.D., Ruzek, J. (2017). Reduction of burnout in mental health care providers using the Provider Resilience Mobile Application. Community Mental Health Journal (53), 452-459.
It seems like everyone is carrying a smartphone these days. Some of the attributes that make these devices an asset to therapy include they’re portable, acceptable, always on (this benefit is probably up for discussion), low cost, programmable, audio and video output, user-friendliness, and ease of use (Boschen, 2008). More and more we are able to recommend and guide our patients through various evidence-based psychotherapies (EBPs) with the help of evidence-based mobile health applications or so-called “apps”. These apps, such as CBT-i Coach and CPT Coach, can supplement our sessions and make it easier for patients to record things such as sleep diaries or thought logs without the burden of remembering to carry around worksheets or journals. It can be difficult for patients to remember to do their homework and to find a place that they feel is safe enough to record their thoughts or behaviors. The accessibility and convenience of apps seems to make it that much easier for patients to engage in treatment and follow through with treatment assignments.
For providers, we now have the same accessibility of a tool that can help us implement self-care practices in our day. We understand the potential consequences of difficulty in managing stressors and the buildup for compassion fatigue, burnout, and secondary traumatic stress, in addition to the negative impact it can have on our personal and professional lives. For many, finding the time for regular self-care through such routines as meditation, yoga, exercise, proper diet, continuing education, or socializing can be difficult to maintain. With a recent development of the Provider Resilience Mobile Application, providers may find another option of implementing and sustaining self-care practices.
The Provider Resilience app, the first app focused on building resilience for health care providers, was developed by the Defense Department’s National Center for Telehealth and Technology (T2). The app allows providers to complete self-assessments of the Professional Quality of Life Scale (ProQOL), to help providers measure their level of burnout and secondary traumatic stress as well as compassion satisfaction.
Let’s take a look at a few screenshots of the app. (You can click on any of the images to see a larger version.) Here is the dashboard, where a provider can find their resilience rating. The resilience rating is based on the ProQOL and burnout score, and responses to the reduction or building of resilience, in addition to the date of your last vacation day. Yes, it also reminds providers to take time off of work. The ProQOL is updated every 30 days while the burnout rating is updated every seven days.
Burnout can also be tracked through provider ratings based on ten affective domains, shown here, describing your approach to work today.
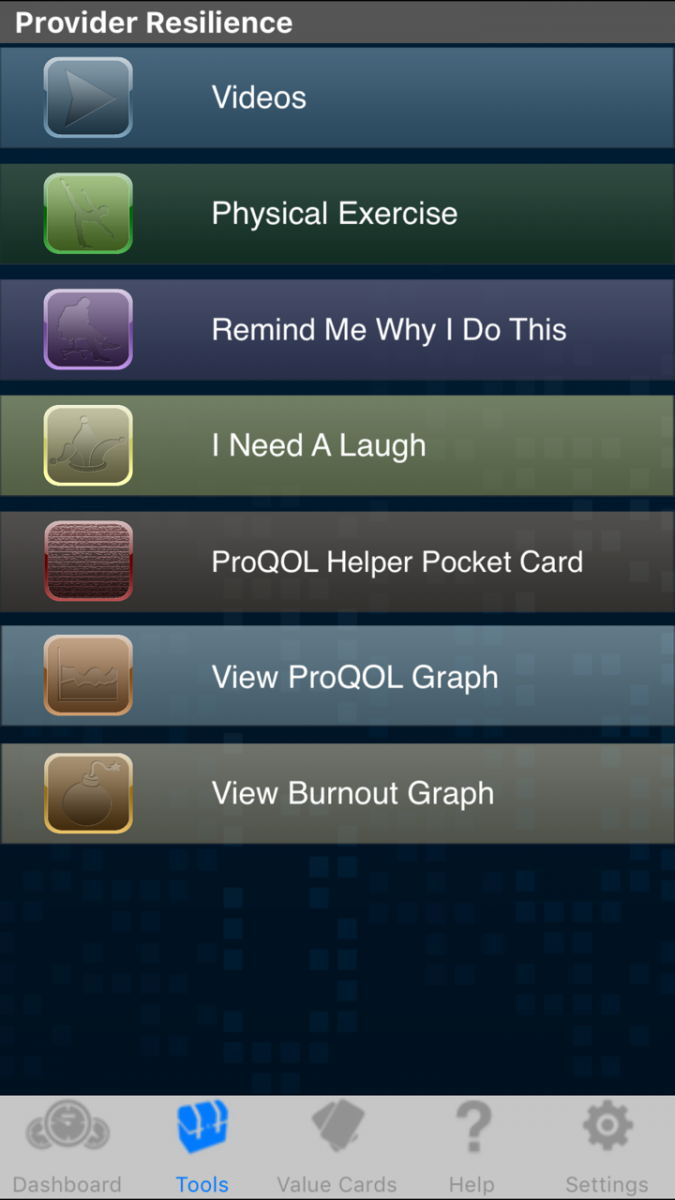 If a provider’s resilience score is low or when looking for strategies to sustain resilience, the app offers a toolbox. These include reminders to take breaks or review positive aspects of work as well as hearing Service members discuss the impact providers have on their lives. This is a great feature; the app specifically focuses on providers who serve Veterans, Service members, and their families.
If a provider’s resilience score is low or when looking for strategies to sustain resilience, the app offers a toolbox. These include reminders to take breaks or review positive aspects of work as well as hearing Service members discuss the impact providers have on their lives. This is a great feature; the app specifically focuses on providers who serve Veterans, Service members, and their families.
Providers can choose from a wide variety of options for self-care, as well as track their ratings over time on the charts.
Here are examples of the Value Cards and Exercises that providers are offered to help increase resilience. 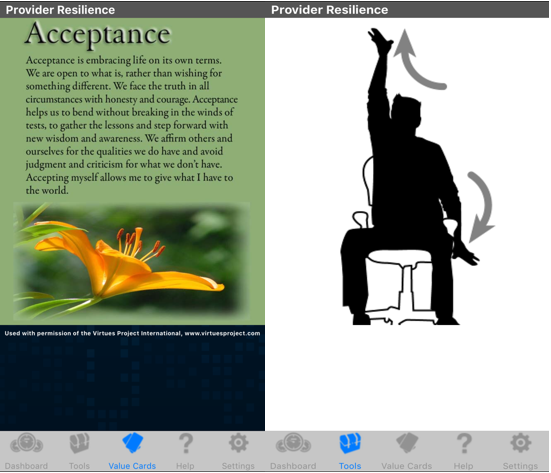
With the development of the Provider Resilience app, we can read up on the latest literature recommending an app’s effectiveness. Recently, Woods et al. (2017), completed a pilot study with 30 outpatient mental health providers who utilized Provider Resilience for a month to examine the usability and effectiveness of the app in reducing provider burnout. The researchers found that not only was the usability considered to be in the “excellent” range with users, but also there was a reduction in burnout (d=0.68) and compassion fatigue (d=0.84). Despite the small sample size, the results are promising in helping to build provider resilience.
There have also been several recent randomized controlled trials (RCT) and reviews suggesting the promising potential of how effective and useful apps are toward psychotherapeutic treatment. One randomized controlled trial (RCT) examined the impact of acceptance and commitment-based apps on stress management which demonstrated the benefits of stress interventions with mobile apps. The use of the app reduced stress and increased general health in middle managers (Ly, Asplund, & Andersson, 2014). Another RCT demonstrated how apps using either behavioral activation or mindfulness might would work well for a depressed population (Ly, et al., 2017). More so, Kuhn et al. (2017) were the first to rigorously evaluate the efficacy of a mobile app for PTSD, PTSD Coach. The results suggested that the app has a potential in helping trauma survivors with PTSD including a recommendation as a first step for those who are not receiving mental health care. A review of evidence-based apps for stress management indicated the great potential for apps in supplementing care (Coulon, Monroe, & West, 2016). Another systematic review concluded that apps are beneficial, feasible, and acceptable for a wide range of psychiatric conditions (Menson, Rajan, & Sarkar, 2017).
Having multiple options for self-care may further help to support providers in sustaining their resilience to continue to service their patients. Providers now have an easy to use app that can help increase resilience by improving levels of burnout and compassion satisfaction. When it may not be as convenient to venture outdoors or be device free, the Provider Resilience app is one more tool among the many that providers can implement into their day. These technological advances are an exciting benefit that will continue to change how we practice both our clinical and self-care tools.
Laura Cho-Stutler, PsyD, is a CBT Trainer working with the Military Training Programs at the Center for Deployment Psychology (CDP) at the Uniformed Services University of the Health Sciences in Bethesda, Maryland.
References
Boschen, M.J. (2008). The use of mobile telephones as adjuncts to Cognitive Behavioral Psychotherapy. Professional Psychology: Research and Practice, 39 (5), 546-552. DOI: 10.1037/0735-7028.39.5.546
Coulon, S.M., Monroe, C.M., West, D.S. (2016). A systemic, multi-domain review of mobile smartphone apps for evidence-based stress management. American Journal of Preventative Medicine, 51(1), 95-101. http://doi.org/10.1016/j.amepre.2016.01.026
Ly, K. H., Asplund, K., & Andersson, G. (2014). Stress management for middle managers via an acceptance and commitment-based smartphone application: A randomized controlled trial. Internet Interventions, Advance online publication. DOI: 10.1016/j.invent.2014.06.003
Ly, K. H., Trüschel, A., Jarl, L., Magnusson, S., Windahl, T., Johansson, R., & Andersson, G. (2014). Behavioural activation versus mindfulness-based guided self-help treatment administered through a smartphone application: A randomised controlled trial. BMJ Open, 4, e003440. DOI: 10.1136/bmjopen-2013-003440
Menson, V., Rajan, T., Sarkar, S. (2017). Psychotherapeutic applications of mobile phone-based technologies: A systematic review of current research and trends. Indian Journal of Psychological Medicine, 39(1),4.
Provider Resilience. National Center for Telehealth & Technology (T2). Provider Resilience, http://t2health.dcoe.mil/apps/provider-resilience, accessed 13 April 2017.
Wood, A.E., Prins, A., Brush, N.E., Hsia, J.F., Bourn, L.E., Earley, M.D., Walser, R.D., Ruzek, J. (2017). Reduction of burnout in mental health care providers using the Provider Resilience Mobile Application. Community Mental Health Journal (53), 452-459.